History
250 Years of Caring for Children
The Department of Pediatrics at Columbia University Irving Medical Center can trace its roots to 1767, when New York was still a British colony. In that year the medical department of King's College, now the Vagelos College of Physicians & Surgeons at Columbia University, was founded. Succeeding generations of Columbia physicians laid the groundwork for what became, over the next 250 years, the modern field of pediatrics. During those two and a half centuries physicians here at Columbia have pioneered many advances in the care of children. Our faculty members established several independent pediatric subspecialties, including pediatric radiology, pediatric neurology, and neonatology. Moreover many diseases and disorders were first described by department members. In the video here pediatric oncologist Dr. Michael Weiner outlines the history of The Babies Hospital, from its founding to the present day. Dr. Weiner is co-author, with Stephen E. Novak, head of Archives & Special Collections at Columbia’s Augustus C. Long Health Sciences Library, of The Babies Hospital of New York from Arcadia Publishing.
Milestones in Pediatrics at Columbia
-
1770
Columbia physicians advance the care of children

Physicians at Columbia University Faculty of Medicine at King’s College describe “blue baby” syndrome, propose a method for intubating infants, and publish the first textbook of obstetrics, A Compendium of the Theory and Practice of Midwifery. They also are at the forefront in recognizing the symptoms, epidemiology, and autopsy findings of diphtheria.
-
1887
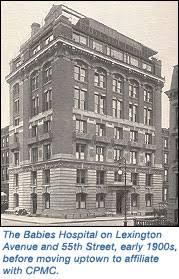
Dr. Sarah McNutt (pictured) and her sister Dr. Julia McNutt found Babies Hospital

Drs. McNutt, Jeannie Smith, Isabella Satterthwaite, and Isabella Banks found Babies Hospital, the first hospital in New York City for children, in a brownstone on Lexington Avenue and 55th Street. The hospital, with only women resident physicians, has 30 beds for sick infants up to three years of age, hence the name of the hospital, “Babies.” Malnutrition is most common diagnosis.
-
1888
Dr. Emmett Holt named medical director

Babies Hospital appoints L. Emmett Holt, who laid the groundwork for the field of pediatrics, as medical director. Dr. Holt observes that nurses are keeping a clipboard at the side of each bed and noting important clinical information on it. He begins adding physician observations to it, giving birth to the medical chart.
-
1891
Babies Hospital uses first incubator in US

The hospital is the first in the US to use incubators, which were developed in France. Until this innovation many premature babies died because they were unable to regulate their body temperature, and the incubator solved this deadly problem.
-
1894
Dr. Holt publishes first manual for mothers

Dr. Holt adapts lecture notes that the head of nursing used to educate parents for his book, The Care and Feeding of Children: A Catechism for the Use of Mothers and Children's Nurses.
-
1897
First pediatrics textbook

Dr. Holt publishes the first modern textbook of pediatrics, Diseases of Infancy and Childhood. This textbook, in its 23rd edition in 2018, is now published as Rudolph’s Pediatrics.
-
1902
Babies Hospital relocates

The new eight-story building on Lexington Avenue has a modern electric elevator, telephone, an X-ray machine, and 80 beds. The hospital also has dedicated departments of pathology, surgery, and radiology.
-
1907
Tay-Sachs disease identified

Neurologist Dr. Bernard Sachs publishes his findings on what was then called “amaurotic family idiocy” and later called Tay-Sachs disease. In 1887 Dr. Sachs had noted the higher incidence of this neurologic condition among Ashkenazi Jews from Eastern Europe.
-
1909
First dedicated ward for preemies
Babies Hospital opens the first ward in the US specifically for premature infants.
-
1922
Pioneers in pediatric radiology

Radiologists at Babies Hospital establish the first pediatric radiology service.
-
1925
Dr. Herbert Wilcox appointed director of Babies Hospital

During the tenure of Dr. Herbert Wilcox Sr. (P&S '02), and under his leadership, Babies Hospital became closely affiliated with Columbia University and Presbyterian Hospital.
-
1929
Babies Hospital relocates again

The hospital, now with 191 beds, moves to Broadway and 167th Street, affiliates with the College of Physicians & Surgeons, and becomes part of Columbia Presbyterian Medical Center. Hospital staff now treat children up to 12 years of age.
-
1930
Dr. Martha Wollstein breaks barriers

Pathologist Dr. Martha Wollstein, whose research showed that mumps is caused by a virus, is elected as the first woman to the American Pediatric Society. Dr. Wollstein also studied polio and pneumonia, and helped to develop an antimeningitis serum.
-
1933
Dr. Rustin McIntosh named Chair

Dr. McIntosh remains department chair until 1960. He fostered a “spirit of doubt and need for inquiry” that led to breakthroughs in the treatments of many childhood diseases.
-
1937
Rare endocrine disease described
Dr. Donovan McCune describes the first case of polyostotic fibrous dysplasia, a rare genetic endocrine disease affecting the bones and pigmentation of the skin, subsequently known as McCune-Albright syndrome.
-
1938
Cystic fibrosis described by Dr. Dorothy Andersen

Pathologist Dr. Dorothy Andersen is the first to recognize the disease cystic fibrosis, and later helps to develop a test to diagnose it.
-
1940
Kasabach-Merritt syndrome described
Dr. Katherine Merritt publishes a case report of an infant with thrombocytopenia with giant hemangioma, subsequently named Kasabach-Merritt syndrome.
-
1942
New treatment of meningitis

Dr. Hattie E. Alexander develops the first treatment of Haemophilus influenzae meningitis, heretofore an infection with case fatality rate of 80%, based on an infusion of an antiserum that she prepared
-
1945
Advances in Radiology

Dr. John Caffey publishes the comprehensive text, Pediatric X-Ray Diagnosis, which establishes the intellectual basis of pediatric radiology. Dr. Caffey also publishes a description of infantile cortical hyperostosis, now known as “Caffey disease,” and shortly after that the first description of “shaken baby syndrome.”
-
1952
Apgar Score created

Anesthesiologist Dr. Virginia Apgar creates a simple scoring method for predicting the health status of newborns, now known as the “Apgar score.” The Apgar score measures five body functions at one minute after birth and again five minutes later to determine whether there is need for life-saving assistance. It has become an international standard of care of neonates.
-
1952
First randomized clinical trial

Neonatologist Dr. William Silverman creates the first randomized clinical trial, which confirmed the harm of adrenocorticotropic hormone in treating retinopathy of prematurity.
-
1953
Sweat test for CF

Building on Dr. Dorothy Anderson's work, Dr. Paul di Sant’Agnese describes elevated sweat chloride in cystic fibrosis, then develops the noninvasive, and now standard, “sweat test” for the diagnosis of this disease.
-
1955
New paradigm for cancer research established

Pediatric hematologist/oncologist Dr. James Wolff is one of the founding members of the Acute Leukemia Chemotherapy Cooperative Study Group A, which pooled patients from several hospitals to ensure a sufficient number of patients to conduct statistically rigorous trials of new therapies. This eventually became the Children’s Oncology Group, now an international network of more than 200 hospitals, universities, and cancer centers. The results of this coordinated approach have spread far beyond pediatric cancers: Many of the drugs that eventually became mainstay treatments for adult cancer were initially tested by this consortium of researchers in pediatric patients.
-
1964
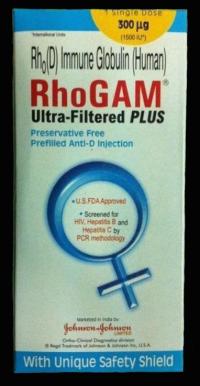
Rh vaccine eradicates Rh disease

Dr. Vincent Freda, an obstetrician, and Dr. John Gorman, director of the blood bank at Presbyterian Hospital, pioneer a vaccine that effectively eradicates Rh disease in newborn children. Rh disease is a form of hemolytic disease of the fetus and newborn that once claimed the lives of nearly 10,000 babies a year in the US. Drs. Freda and Gorman receive the 1980 Albert Lasker Clinical Medical Research Award in recognition of their work.
-
1964
Prognostic guidelines for retinoblastoma

Dr. Algernon Reese, founder of the field of ophthalmic oncology, develops the Reese-Ellsworth classification of retinoblastoma to predict a patient’s prognosis after treatment with radiation.
-
1964
Breaking through the glass ceiling

Dr. Hattie Alexander is named president of the American Pediatric Society, and is one of the first women to head a national medical association.
-
1969
Dr. Welton Gersony publishes the first description of pulmonary hypertension of the newborn.
-
1973
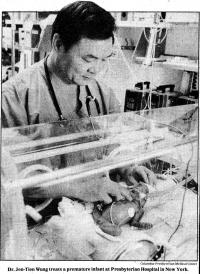
Nasal CPAP improves future for preemies

Dr. Jen-Tien Wung pioneers the use of non-invasive nasal continuous positive airway pressure (CPAP) therapy to manage respiratory problems in premature infants, with the support of Drs. Stanley James, John Driscoll, other colleagues, and NICU nursing staff. CPAP is shown to reduce the need for invasive mechanical ventilation and its complications and to improve survival rates, especially among extremely low birthweight infants.
-
1976
Dr. Michael Katz named Chair

Pediatrician and noted tropical medicine specialist Dr. Michael Katz is named chair of the department. During his tenure specialists at Columbia perform the first pediatric heart transplant, describe the syndrome of persistent fetal circulation, and develop continuous positive alveolar pressure (CPAP) for premature infants. Dr. Katz is a consultant to the World Health Organization, among many other organizations here and abroad, and from 1992 to 2018 is senior vice president for research and global programs, then senior advisor, transdisciplinary research, of the March of Dimes Foundation.
-
1982
A pediatrician leads the America Thoracic Society

Dr. Robert Mellins is the first and only pediatrician to be appointed president of the American Thoracic Society. Dr. Mellins, a founding father of the field of pediatric pulmonology, was an international authority in the field of pediatric asthma and a career-long advocate for multidisciplinary research and patient care who welcomed into his laboratory and clinics trainees from disciplines as widespread as allergy, anesthesiology, engineering, health education, psychology, and nutrition.
-
1982
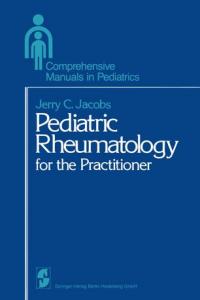
First textbook of pediatric rheumatology

Dr. Jerry Jacobs, a leading authority on rheumatoid arthritis in children, publishes Pediatric Rheumatology for the Practitioner, a Springer Verlag book in the series for practitioners, edited by Dr. Katz.
-
1984
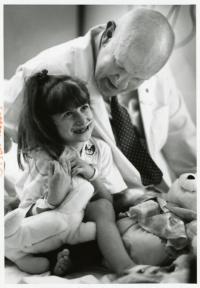
Successful heart transplant in a child

Columbia surgeons Keith Reemtsma, MD and Eric Rose, MD perform one of the first successful pediatric heart transplants at Columbia. Pediatric heart transplants are now standard, and surgeons now perform about 30 at NewYork-Presbyterian/Columbia each year, more than any other center.
-
1992
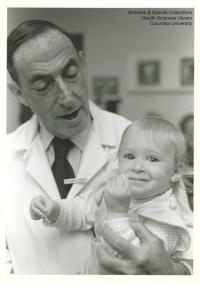
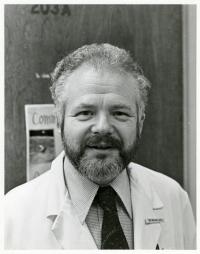
Dr. John Driscoll named department chair

Photo credit: Archives & Special Collections, Health Sciences Library, Columbia University
Neonatologist Dr. John Driscoll, who had directed the NICU since 1971, is named chair of Pediatrics. Under his leadership, the NICU gained international recognition for its innovative approaches. During Dr. Driscoll’s 15-year tenure as chair, he was instrumental in the construction of the new Morgan Stanley Children’s Hospital. He retired in June 2007.
-
1995
FDA licenses chickenpox vaccine

Based on the research of Dr. Anne Gershon, who studied its safety and efficacy, the varicella zoster vaccine is licensed for use in the US. By 2005 the number of chickenpox cases has dropped by 90 percent, and chicken pox-related deaths in children by 97 percent. In 2013 Dr. Gershon receives the Albert B. Sabin Gold Medal from the Sabin Vaccine Institute.
-
2008
Dr. Lawrence Stanberry appointed Chair

Dr. Lawrence Stanberry, a world-renowned virologist and prolific author, is appointed department chair. Under his leadership the department expands its NIH funding and endowment, creates a faculty development and mentorship program and Children’s Board, and enters the era of precision medicine with the Precision in Pediatric Sequencing (PIPseq) program. The department establishes programs in Global Health Security and Diplomacy, complex care coordination for children with multi-system illnesses, and comprehensive obesity prevention and treatment. The department also opens the Milstein Infant Cardiac Unit, the first such dedicated infant unit in world; the Phyllis and Ivan Seidenberg Center for Children’s Digestive Health; and the Neuro Intensive Care Unit. Dr. Stanberry retires in 2018.
-
2018
Genetic causes of certain rare diseases identified

While diagnosing and treating children with rare disorders through the Discover Program, clinical geneticist Wendy Chung MD, PhD identifies 40 novel genes in diseases including pulmonary hypertension, congenital heart disease, congenital diaphragmatic hernia, and autism. Dr. Chung led the pivotal study of newborn screening for spinal muscular atrophy.
-
2018
Dr. Jordan Orange appointed Chair of Pediatrics

Dr. Jordan Orange, an international leader in pediatric primary immunodeficiency, is credited with defining a new class of diseases known as natural killer cell deficiencies. Throughout his career Dr. Orange has blended a commitment to pediatric clinical care with a focus on basic and translational research.